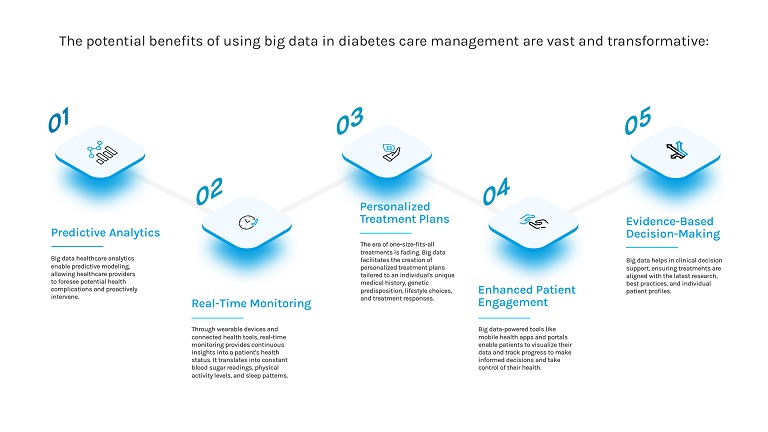
Researchers are turning to big data to better understand how diabetes develops and spreads. By analyzing large, diverse datasets from sources such as electronic health records and wearable devices, they are identifying trends that can guide prevention efforts and improve care. Industry influencers such as Joe Kiani, founder of Masimo and Willow Laboratories, are seeing how the shift toward data-informed strategies can help address chronic conditions more effectively.
As global diabetes rates continue to rise, this approach is offering a clearer view of how the disease varies across regions and populations. It is also helping public health officials, clinicians and policymakers respond with more timely, targeted interventions.
A New Lens in A Growing Health Crisis
Unlike limited clinical trials or survey-based studies, big data draws from sources like electronic health records, insurance claims, mobile health apps, wearable devices and even social determinants of health. These data points collected over time and across geographies create a fuller picture of how diabetes affects individuals and populations.
This more dynamic approach allows scientists to monitor diabetes-related trends in the near real-time. They can detect regional spikes, correlate disease progression with lifestyle habits and track how risk factors vary between age groups or communities. These capabilities are helping public health officials, providers and researchers act faster and smarter.
Mapping Risk Factors Across Populations
One of big data’s greatest strengths is its ability to identify and compare risk factors across diverse populations. By aggregating medical, environmental, genetic and behavioral information, analysts can determine how different combinations of variables contribute to diabetes onset.
For example, in one region, a spike in Type 2 diabetes might be tied to limited access to fresh food. In another, the root cause may be a lack of preventive care or sedentary lifestyles. Big data helps uncover these relationships on a scale, enabling more precise interventions tailored to specific community needs.
It also challenges old assumptions. Factors once believed to be universally high-risk are now being reevaluated in the context of other conditions, lifestyles or environments. This deeper understanding helps refine risk models and prioritize interventions for those most in need.
Real-Time Monitoring Through Wearables and Apps
Consumer health technology, particularly wearable devices and mobile health apps has opened a new chapter in big data collection. People with diabetes can now track glucose, sleep, diet, activity and medication adherence in real-time. When shared anonymously and securely, this data contributes to large-scale health databases that power new insights.
With millions of users logging thousands of interactions daily, these platforms create a volume and richness of data that clinical environments simply can’t match. Researchers can observe how glucose levels respond to specific meals, how stress affects insulin response or how seasonal changes impact overall disease management. Patterns that used to take years to verify can now be spotted in weeks or even days, offering quicker paths to innovation.
Predictive Modeling and Preventive Strategies
Big data doesn’t just describe what’s happening; it predicts what might happen next. Advanced algorithms can sift through layers of data to identify people at high risk for developing diabetes, sometimes before symptoms even appear.
This predictive power has enormous potential. Health systems can use it to target early screenings, personalize lifestyle recommendations and allocate resources more effectively. Employers and insurers are also beginning to adopt these tools to design proactive rather than reactive wellness programs.
These advancements in predictive modeling reflect a larger movement toward early detection and frictionless care. As technology leaders work to simplify chronic disease management, Joe Kiani put it this way: “Big data is giving us a clearer picture of diabetes on a global scale, helping researchers spot trends, identify risk factors, and tailor prevention efforts like never before.” That commitment underscores the value of using data to intervene earlier, personalize care, and support patients before complications arise.
Integrating Social and Environmental Data
Beyond personal and clinical data, social and environmental factors play a large role in diabetes outcomes. Big data platforms are increasingly integrating information such as income levels, education, neighborhood access to healthy food and exposure to environmental pollutants.
These broader insights help health organizations address the root causes of diabetes, not just its symptoms. In areas with high disease rates, data may reveal that improving walkability, expanding grocery access or providing public transportation could directly impact reducing new diagnoses.
This cross-sector integration reflects the shift toward treating diabetes as a social, economic and public health challenge, one that medicine alone cannot solve.
Ethical Considerations and Data Privacy
With so much health data being collected, protecting people’s privacy has never been more important. Tech leaders and public health officials face the tough task of making sure data is used responsibly, without compromising individual rights.
To maintain trust, organizations must invest in robust data encryption, clear consent protocols and transparent data-use practices. The promise of big data depends not only on its scope but also on how responsibly it’s handled.
Case Studies in Action
Several global initiatives are already demonstrating the power of big data in diabetes care. In India, for example, researchers used mobile health data from rural clinics to map out Type 2 diabetes prevalence across regions that previously lacked formal reporting. In the U.S., insurance providers are using predictive analytics to flag high-risk members and offer early intervention programs.
Some digital health companies are even working with pharmacies and grocery chains to merge prescription histories with food purchasing data, uncovering new links between diet patterns and glucose spikes. These collaborations show that big data can drive both innovation and practical application at every level of care.
A Smarter Path Toward Diabetes Prevention
The rise of big data in healthcare is changing how we understand, predict and respond to diabetes globally. It provides the clarity needed to move beyond one-size-fits-all strategies, allowing for more targeted, effective and equitable approaches to disease prevention and management.
As technology continues to grow more complex, leaders remain at the forefront of pushing healthcare toward systems that simplify complex challenges through smart solutions. By leveraging big data responsibly, the future of diabetes care could become not only more precise but more personal, giving individuals and communities the tools they need to stay ahead of the disease.